- Table of contents
-
- Technological Device
- Keywords
-
- Safety at home
Do you know that people with dementia are at a high risk of falls?
The advancement of the technologies offers a lot of help with the care process.
An example in this field is the Bed Sensor Pad.
Apps

What is the idea of this tool?
It alerts the caregiver when pressure is released from the pad. The pad can be put on the seat of a chair, and the monitor will alert the caregiver when the patient stands up or leaves the chair.
Recommendation
A device like this is safe to use. People with dementia and their caregivers can feel comfortable and will avoid risks
Do you know that people with dementia are at a high risk of falls?
Falls and unstable balance are a major contributor to the high mortality rates among the elderly, and contribute substantially to the limitation of mobility and premature entry into assisted living. The data shows us that among the elderly hospitalized after a fall, only half survive for more than a year. Although most of these falls do not cause major injuries, about 5% cause a fracture or require hospitalization. In addition, the associated complications increase significantly with age and double in people over 75 years old.
In general, the functional conditions that facilitate falls are loss of muscle strength, difficulty walking and balancing, muscle weakness, which in subjects with dementia then creates an even greater risk.
More in detail, considering the risk of falling as a multifactorial complex, factors such as balance, gait, vision, psychosocial and environmental factors and dementia progression must be taken into account.
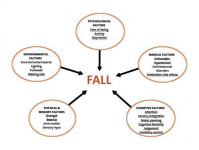
People living with forms of dementia such as Parkinson's disease, Lewy Body Dementia or Vascular Dementia are more prone to movement disorders.
A multidisciplinary approach to the problem suggests that cognitive assessment, with a focus on executive functions and gait assessment should be integrated into risk assessment.
Strategies used may include:
- the use of walking aids on the basis of psychophysical characteristics;
- training programs that identify anomalies in gait, as well as strength and balance;
- specific interventions to improve attention, planning skills, problem solving and cognitive flexibility aimed at improving walking especially in the planning and execution of complex routes;
- the assessment of the patient's risk attitude, judgment and inhibitory control;
- a good communication strategy with the person by the caregiver. It is important to use clear and simple language, with short sentences, to suggest one instruction at a time making sure that it has been received, to give time to receive the message, encourage and motivate them, at the same time monitoring their gestures and expressions so as not to instill fear or confusion. Meanwhile make sure of the person's attention, encourage eye contact, reduce possible environmental distractions during communication.
In addition, environmental interventions within the home, such as:
- facilitated viewing and concentration on relevant details, on lighting and contrast; use of aids such as night lights or switches visible in the dark, lighting specific spaces (such as doors, wardrobes); avoid objects with too blurred contours;
- obstacles and dangerous objects must be removed from the ground, carpets or moving objects on the floor, holes or leaks of liquid on surfaces must be avoided, sharp edges on surfaces avoided and low, dangerous and unstable furniture;
- objects of common use must be usable, kept as close as possible, if possible, put labels on cabinets and other objects to facilitate recognition;
- use appropriate, comfortable and non-slip footwear;
- avoid exposure to sudden and intense sounds that can scare people and lead to sudden runaway behaviors.
Finally, a huge help could come from the use of technology such as the Bed Sensory Carpet, which can be placed on people with dementia’s bed or chair. The monitor will alert the caregiver when the patient stands up or leaves the chair. It can contribute to the safety and autonomy of the person, who can remain alone in a room for short periods of time in safe conditions.
References
Fernando E. et al (2017), Risk Factors Associated with Falls in Older Adults with Dementia: A Systematic Review. Physiotherapy Canada, Spring 2017; 69(2): 161–170.
Zhang W. Et al (2019), Review of Gait, Cognition, and Fall Risks with Implications for Fall Prevention in Older Adults with Dementia. Dementia and Geriatric Cognitive Disorders 2019 ;48:17–29
ISS Epicentro, Le cadute negli anziani, da https://www.epicentro.iss.it/incidenti-domestici/rischi-cadute-anziani#7
Shaw, Fiona. (2003). Falls in Older People with Dementia. Geriatrics & Aging, p 37-40.
Alzheimer Society of Manitoba, Reducing risk of falls for people with Dementia, da https://www.alzheimer.mb.ca/wp-cont...014-Dementia-Fall-Risk-Checklist-template.pdf, ultimo accesso 28/01/2022